March 20, 2023
In the best of times, Family Medicine is complicated. It’s not just runny noses and sore throats by any stretch of the imagination.
On an average day, family physicians see 20 or more patients, ranging from newborns to senior citizens. They take care of individuals with multiple chronic diseases, such as hypertension and diabetes; they take care of patients with difficult behavioral health disorders like depression, anxiety, and substance use disorder; and they take care of urgent or emergent issues from broken bones to chest pain. Most of the adults that family physicians treat don’t just have one issue, but multiple illnesses or chronic diseases, further complicating their care.
Family Medicine is not for the faint of heart, nor is it for individuals with limited training— unless they are working in teams.
As we wrestle with health care coming out of a pandemic, it’s time to refocus on patient safety as we develop the teams of tomorrow. Any team is only as strong as its leader. A family physician is traditionally the leader of the team in a medical home. This distinction is in place for many reasons, including breadth of education, depth of training, adeptness at patient safety, the efficiency of managing resources, promotion of equal access to medical care, and cultivation of the doctor-patient relationship. More than ever, we must concentrate on improving outcomes while controlling costs. Family physicians are uniquely qualified to do just that.
Family physicians are trained to deal with multiple complicated diagnoses. They are constantly investigating underlying issues to make the difficult diagnosis. Family physicians have the training and experience to do just that. Not all health care providers do.
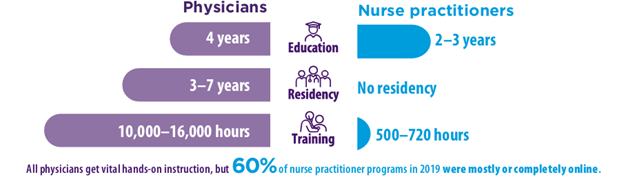
To become a family physician, you must complete a four-year undergraduate degree, four more years in medical school, and a minimum of three years of residency. Medical school and residency governing bodies have numerous specific requirements. In residency, family physicians work side by side with experienced faculty members, seeing patients in both outpatient and inpatient settings. For the first year of residency, an experienced family physician provides oversight for every single patient. And these experienced faculty members remain highly engaged with patient care through the second and third years of residency as well.
By the time a family physician can begin practicing on their own, they have completed 12,000 to 16,000 hours of clinical training over the course of medical school and residency (a minimum of seven years in addition to college degrees).
In contrast, nurse practitioners only receive two years of training after college, their training can be inconsistent, and they are only required to complete 500 to 1,500 hours of direct clinical experience. The difference between their training and that of family physicians is substantial. We value our nursing colleagues. However, to ensure high-quality, cost-effective medical care, you simply cannot replace a family physician with a nurse practitioner. They need physician involvement, as does the patient.
To think about medical care in this new era, it is imperative that the physician — due to their education, experience, quality of care, and cost-effectiveness — lead the healthcare team.
The NC Patient Safety Coalition is an alliance of medical professionals that advocate for physician-led health care that protects patient safety. Learn more on our website at www.ncpatientsafety.com, and follow us on Twitter @NCPatientSafety and Facebook www.facebook.com/NCPatientSafety.